UNIT 3 ADMISSION
A 28y old male came to the opd with chief complaints of fever since 10 to 25 days and SOB since 5 to 6 days.
Patient was apparently asymptomatic 15 days back then developed fever which was incidious in onset and non progressive. It was associated with chills and dry cough. Not associated with cold.
C/O SOB since 5 to 6 days that progressed from grade 2 to grade 3. Not associated with pedel edema and loose stools.
No h/o bleeding manifestations, bleeding gums, malena, hemoptysis, hemetemesis.
PAST HISTORY:
No h/o similar complaints of in the past. No h/o DM, HTN, CAD, Asthma, TB.
PERSONAL HISTORY :
Patient has a mixed diet with decreased appetite and adequate sleep. Patient has constipation. Normal bladder filling and micturition. No addictions.
No significant family history.
GENERAL EXAMNATION:
Patients is c/c/c. No pallor, icterus, cyanosis, clubbing, Vital2s lymphadenopathy, pedel edema.
VITALS:
temp: 101 F
PR: 98 bump nd
RR: 18 cpm.
BP: 90/70 mmhg.
SPO2: 96% at RA.
RS: BAE +, NVBS
CVS: S1 ans S2 heard. No murmurs.
P/A: soft and non-tender.
CNS: No focal deformities.
INVESTIGATIONS:
1) SERUM ELECTROLYTES:
NA: 134.
K: 4.6
CL: 96.
2) Serum Creatinine: 1.1
3) Serum Urea: 32 mg/dl
4) LFT:
TB: 0.94
DB: 0.3
SGOT: 117
SGPT: 114
AP: 183
TP: 5.7
A: 2.3
A/G RATIO:.0.68
5) Serology: negative
6) HEMOGRAM:
Hb: 11.9
TC: 7,700
N/L/E/M/B: 80/16/2/2/0
PLT: 2.2 lakh
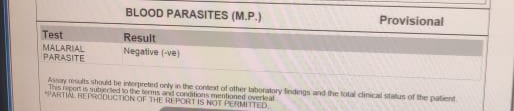
7) MP STRIP : Negative.
8) CUE : normal.
9) USG: NORMAL.
10) RAPID DENGUE: Negative.
PROVISIONAL DIAGNOSIS :
VIRAL PYREXIA UNDER EVALUATION.
HEMOGRAM (20/10/21)
22/10/21
SERUM ELECTROLYTES (20/10/21)
LFT (20/10/21)
CUE (20/10/21)
SERUM CREATININE
RAPID DENGUE TEST
SEROLOGY: NEGATIVE
USG abdomen
TREATMENT:
DAY 1
1)IV Fluids NS and RL -100 ml/hr
2)inj optineurin 1 amp in 100 ml/hr IV bd
3)inj Monocef 1gm IV bd
4)Tab.Doxycyline 100 mg po bd
5)inj pan 40 mg IV od BBF
6)inj zofer 4 mg IV SoS
7) inj Neomol 1 gm iv SoS
8)Tab .Dolo 650 mg po sos
9 ) Bp temp,PR monitoring 6 th hourly ,inform SOS
DAY 2
1)IV Fluids NS and RL -100 ml/hr
2)inj optineurin 1 amp in 100 ml/hr IV bd
3)inj Monocef 1gm IV bd
4)Tab.Doxycyline 100 mg po bd
5)inj pan 40 mg IV od BBF
6)inj zofer 4 mg IV SoS
7) inj Neomol 1 gm iv SoS
8)Tab .Dolo 650 mg po sos
9 ) Bp temp,PR monitoring 6 th hourly ,inform SOS
FEVER CHART
SOAP NOTES
DAY 1
AMC bed 2
21/10/21
S: fever present
O: pt is conscious coherent and cooperative
O/E
PR: 72 BPM
BP: 80/60 mmHg
RR :18 Cpm
Temp:98.6F
CVS: S1,S2 heard
RS NVBS +
P/A
Soft non tender
Bowel sounds+
CNS : NFD
A:viral pyrexia under evaluation
P:
1)IV Fluids NS and RL -100 ml/hr
2)inj optineurin 1 amp in 100 ml/hr IV bd
3)inj Monocef 1gm IV bd
4)Tab.Doxycyline 100 mg po bd
5)inj pan 40 mg IV od BBF
6)inj zofer 4 mg IV SoS
7) inj Neomol 1 gm iv SoS
8)Tab .Dolo 650 mg po sos
9 ) Bp temp,PR monitoring 6 th hourly ,inform SOS
DAY 2
AMC bed 2
22/10/21
S: no present complaints
O: pt is conscious coherent and cooperative
O/E
PR: 66 BPM
BP: 90/60 mmHg
RR :18 Cpm
Temp:98.6F
CVS: S1,S2 heard
RS NVBS +
P/A
Soft non tender
Bowel sounds+
CNS : NFD
A:viral pyrexia under evaluation
P:
1)IV Fluids NS and RL -100 ml/hr
2)inj optineurin 1 amp in 100 ml/hr IV bd
3)inj 6 Monocef 1gm IV bd
4)Tab.Dt4oxycyline 100 mg po bd
5)inj pan 40 mg IV od BBF
6)inj zofer 4 mg IV SoS
7) inj Neomol 1 gm iv SoS
Tat4eb .t4Dolo 650 mg po sos
9 ) Bp temp,PR monitoring 6 th hourly ,inform SOS















Comments
Post a Comment